Root canal treatment is one of the most common dental procedures performed worldwide, yet many patients have little understanding of how their tooth will appear afterward. When your dentist recommends a root canal, they’re essentially saving your natural tooth from extraction while removing the infected or damaged pulp inside. This procedure has evolved significantly over the years, with modern techniques focusing not just on functionality but on maintaining the natural appearance of your tooth as well.
The external appearance of a tooth immediately after a root canal often surprises patients. In most cases, the tooth looks remarkably similar to how it did before the procedure, especially if a temporary filling is placed. However, there are subtle changes that occur both immediately and over time that patients should understand. These changes are normal and typically don’t affect the tooth’s function or your smile aesthetics, especially with proper restoration.
The tooth undergoes significant transformation during root canal therapy. The dentist removes all the living tissue (pulp) from inside the tooth, including the nerve and blood vessels. This space is then cleaned, shaped, disinfected, and filled with a rubber-like material called gutta-percha. While this internal change doesn’t directly affect the external appearance, it does make the tooth more brittle over time, which is why most dentists recommend placing a crown after the root canal procedure.
Patients often worry that their tooth will look “dead” or noticeably different after a root canal. This misconception couldn’t be further from the truth. With modern dental techniques and materials, root canal-treated teeth can blend seamlessly with your natural smile. The key factors that determine the final appearance include the tooth’s initial condition, the extent of damage before treatment, the quality of the root canal procedure, and the type of restoration placed afterward.
The journey of a tooth through root canal treatment and restoration is fascinating from both a biological and aesthetic perspective. Understanding what to expect can alleviate anxiety and help patients make informed decisions about their dental care. As we explore the various aspects of post-root canal tooth appearance, you’ll gain valuable insights into this common yet often misunderstood dental procedure.
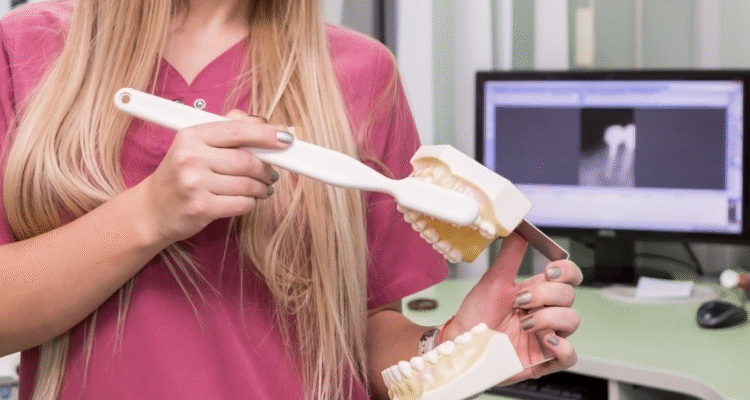
The Root Canal Procedure: A Brief Overview
A root canal procedure, also known as endodontic therapy, is designed to save a tooth that has become infected or severely decayed. During this treatment, your dentist or endodontist will first administer local anesthesia to ensure your comfort. They then create a small opening in the crown of the tooth to access the pulp chamber. Using specialized instruments, they carefully remove the infected or damaged pulp, clean and shape the canals, and then fill them with gutta-percha. Finally, the access point is sealed with a temporary or permanent filling.
Immediate Post-Procedure Appearance
Immediately after your root canal, your tooth will look much the same as it did before the procedure, with one notable difference: the presence of a temporary filling. This filling is typically made of a soft material that’s easy for your dentist to remove when you return for your permanent restoration. The tooth itself might feel slightly different due to the absence of nerve tissue, but visually, it should blend in with your surrounding teeth. Some patients notice minimal swelling around the treated area, but this usually subsides within a few days.
Long-Term Changes in Tooth Structure
Over time, a root canal-treated tooth may undergo subtle changes in structure. Without blood supply, the tooth can become slightly more brittle than your vital teeth. This increased brittleness isn’t visible externally but makes the tooth more susceptible to fracture if not properly restored with a crown. Additionally, some teeth may gradually develop a slight grayish or yellowish tint over years, particularly if the tooth was severely damaged before treatment or if the restoration materials used aren’t perfectly color-matched to your natural teeth.
The Role of Dental Crowns in Post-Root Canal Aesthetics
Dental crowns play a crucial role in both protecting and enhancing the appearance of root canal-treated teeth. A crown is a custom-made cap that covers the entire visible portion of the tooth. Modern crowns are crafted from materials like porcelain, ceramic, or porcelain-fused-to-metal, which can be precisely color-matched to your surrounding teeth. When properly designed and placed, a crown can make your root canal-treated tooth indistinguishable from your natural teeth. In fact, many patients find that their crowned tooth looks better than it did before the root canal, especially if the original tooth was discolored or damaged.
Common Misconceptions About Root Canal Treated Teeth
There are numerous misconceptions surrounding the appearance of teeth after root canal treatment. One of the most persistent myths is that root canal-treated teeth always turn dark or black. While this was more common decades ago when different materials were used, modern techniques have largely eliminated this issue. Another misconception is that root canal-treated teeth eventually fall out. In reality, with proper care and restoration, these teeth can last a lifetime. Some patients also worry that their treated tooth will look obviously different from their natural teeth, but with today’s advanced dental materials and techniques, this is rarely the case.
Maintaining Your Root Canal Treated Tooth
Proper maintenance is essential for preserving both the function and appearance of your root canal-treated tooth. Good oral hygiene practices including brushing twice daily, flossing regularly, and using an antiseptic mouthwash can help prevent decay in the surrounding tooth structure. Regular dental check-ups allow your dentist to monitor the condition of the restoration and the underlying tooth structure. Additionally, if you grind your teeth or participate in contact sports, wearing a protective night guard or sports guard can help prevent damage to your restored tooth. Remember that while the tooth itself no longer has nerves, the surrounding tissues do, so maintaining gum health is crucial for the overall success of your root canal treatment.
Signs of a Successful Root Canal Treatment
Identifying a successful root canal treatment involves both visual examination and functional assessment. When performed correctly, a root canal should alleviate pain, resolve infection, and preserve the natural tooth structure while maintaining a natural appearance. The success of the procedure isn’t immediately apparent in all cases, as complete healing of the surrounding tissues can take several months. However, there are specific indicators that dental professionals look for to determine if a root canal has been successful.
From a visual standpoint, a successfully treated tooth should appear healthy and integrated with your surrounding dentition. There should be no visible signs of infection, such as swelling, redness, or drainage around the gumline. The tooth should feel stable and firm, with no mobility when gently touched. When restored with a crown or filling, the margins should be tight and sealed, with no visible gaps where bacteria could penetrate. The color of the tooth should remain consistent with your natural teeth, though some minor changes might occur over time.
Color Changes: What’s Normal and What’s Not
After a root canal, some color changes in the tooth can occur, and it’s important to distinguish between normal variations and signs of potential problems. Slight yellowing or graying over several years is relatively common and usually doesn’t indicate treatment failure. This occurs because the tooth no longer has a blood supply and the internal tubules may become more mineralized over time. However, significant darkening shortly after treatment, especially if accompanied by pain or swelling, could indicate problems with the procedure or the development of new decay. In such cases, consult your dentist promptly to evaluate the situation.
Structural Integrity After Root Canal
The structural integrity of a root canal-treated tooth is crucial for its long-term success. While the tooth may look normal externally, the removal of pulp tissue makes it more brittle than vital teeth. This is why most dentists recommend placing a crown after root canal treatment, especially for posterior teeth that endure significant chewing forces. A properly restored tooth should feel solid when you bite down, with no unusual movement or sensation. If you notice your tooth feels loose or moves when touched, this could indicate a problem with the restoration or underlying bone support and warrants immediate dental attention.
Pain and Sensitivity: Post-Treatment Expectations
It’s normal to experience some mild discomfort or sensitivity for a few days after a root canal procedure, especially when chewing or applying pressure to the treated tooth. This sensitivity typically diminishes as the surrounding tissues heal. However, persistent pain that lasts beyond a week or two, severe pain that wakes you at night, or pain that returns after initially subsiding could indicate treatment complications. Successful root canal treatment should ultimately result in a tooth that is comfortable to use for normal chewing and doesn’t cause spontaneous pain. If you’re experiencing ongoing discomfort, your dentist may need to evaluate the tooth for potential issues.
X-Ray Evidence of a Well-Performed Root Canal
Dental X-rays provide crucial information about the success of a root canal treatment that isn’t visible to the naked eye. On a radiograph, a successfully treated tooth will show complete filling of the root canal spaces with gutta-percha, extending to the tip of the root but not beyond. There should be no visible spaces where bacteria could potentially grow. Over time, the bone around the root tip should appear healthy and show signs of healing if there was pre-existing infection. Your dentist will typically take follow-up X-rays at six months and one year post-treatment to confirm that the healing process is progressing normally.
Functional Assessment of the Treated Tooth
Beyond appearance, the functional success of a root canal-treated tooth is paramount. A successfully treated tooth should function just like your natural teeth for chewing and biting. You should be able to eat normally without pain or sensitivity to temperature. The tooth should not feel “different” from your other teeth during normal use. While the absence of nerve tissue means you won’t feel temperature changes in that specific tooth, the surrounding periodontal ligament provides sufficient sensory feedback for normal function. If your restored tooth feels high when you bite down or causes discomfort during normal chewing, your dentist may need to adjust the bite or evaluate the restoration.
Potential Complications and Their Visual Indicators
While root canal treatments have a high success rate, complications can occasionally occur. Being able to recognize the visual indicators of potential problems can help you seek timely intervention and preserve your tooth. These complications range from minor aesthetic issues to more serious conditions that could jeopardize the tooth if left untreated. Understanding what to watch for empowers patients to take an active role in their post-treatment care.
The most common complications following root canal treatment include reinfection, fracture of the tooth, discoloration, and problems with the restoration. Each of these issues presents with distinct visual and symptomatic clues that, when recognized early, can often be addressed before they become more serious. Regular dental check-ups are essential for identifying problems that might not be visible or symptomatic in their early stages, but knowing what to look for between visits can make a significant difference in the long-term outcome of your treatment.
Discoloration Issues and Solutions
Tooth discoloration after root canal treatment can occur for several reasons. The most common cause is the breakdown of blood products that were present in the tooth before treatment, which can stain the dentin from the inside. Additionally, some root canal filling materials used in the past contained components that could cause darkening over time. Modern techniques have largely eliminated this issue, but if you notice your tooth becoming significantly darker, several solutions are available. These include internal bleaching (where a whitening agent is placed inside the tooth), veneers, or replacement of the restoration with a crown that better matches your natural tooth color.
Cracks and Fractures: Identifying At-Risk Teeth
Root canal-treated teeth are more susceptible to cracks and fractures due to their increased brittleness. Visual indicators of a cracked tooth include:
- Sudden pain when chewing or biting
- Sensitivity to temperature changes
- Pain that comes and goes
- Visible lines on the tooth surface
- Swelling of the gum around the affected tooth
While not all cracks are visible to the naked eye, if you notice any of these symptoms, especially if they develop months or years after your root canal, consult your dentist promptly. Early intervention can sometimes save the tooth, but untreated cracks can lead to vertical root fractures that often result in tooth loss.
Reinfection Signs to Watch For
Reinfection of a root canal-treated tooth, though uncommon, can occur and presents specific visual and symptomatic signs. Watch for:
- The appearance of a pimple or bump on the gums near the treated tooth
- Swelling that returns after initial healing
- Darkening of the tooth beyond normal aging
- Tenderness when touching the gum around the tooth
- A bad taste or odor coming from the tooth
These symptoms indicate that bacteria may have re-entered the tooth, possibly through an undetected crack, decay under the restoration, or incomplete initial cleaning of the root canals. If you observe any of these signs, schedule an appointment with your dentist as soon as possible, as reinfection requires prompt treatment to prevent abscess formation and potential tooth loss.
Failed Root Canal: Visual and Symptomatic Clues
A failed root canal presents with both visual and symptomatic clues that should not be ignored. The most obvious symptom is the return of pain in the treated tooth, especially if it’s similar to the pain you experienced before the procedure. Visually, you might notice swelling or redness in the gums around the tooth, or the development of a gum boil (a small pimple-like bump that may release pus). On X-rays, your dentist would look for dark areas around the root tip, indicating bone loss due to persistent infection. Other signs include increased mobility of the tooth, sensitivity to pressure, or the development of a sinus tract (a small channel from the infection to the gum surface). If you experience any of these symptoms, your dentist may recommend root canal retreatment or other interventions to address the problem.
When to Seek Professional Evaluation
Knowing when to seek professional evaluation for your root canal-treated tooth can make the difference between saving and losing the tooth. Schedule an immediate dental appointment if you experience:
- Severe pain that doesn’t respond to over-the-counter pain medication
- Significant swelling in your face, jaw, or gums
- Difficulty breathing or swallowing (this requires emergency care)
- A fever along with tooth pain
- A loose tooth that wasn’t loose before
- Visible cracks or fractures in the tooth
Schedule a routine evaluation if you notice milder symptoms like occasional pain when chewing, sensitivity to temperature, or changes in the appearance of your gums around the treated tooth. Remember that early intervention is always preferable when dealing with potential complications of root canal treatment.
Long-Term Care and Maintenance of Root Canal Treated Teeth
The longevity of a root canal-treated tooth depends significantly on how well it’s cared for after the procedure. While the root canal itself removes the infected pulp and eliminates the source of infection, the tooth still requires diligent maintenance to remain functional and aesthetically pleasing. Proper care not only preserves the treated tooth but also protects your investment in the procedure, as root canals followed by appropriate restoration represent a significant commitment of time and resources.
Many patients mistakenly believe that once a tooth has had a root canal, it no longer requires the same level of care as natural teeth. This couldn’t be further from the truth. In fact, root canal-treated teeth often need more attentive care because they’re more brittle and lack the natural defense mechanisms of vital teeth. The good news is that with proper maintenance, including good oral hygiene, regular dental visits, and appropriate protective measures, root canal-treated teeth can last a lifetime, functioning just like your natural teeth.
Daily Oral Hygiene Practices
Maintaining excellent oral hygiene is crucial for the long-term success of your root canal-treated tooth. Brush your teeth at least twice daily using a soft-bristled toothbrush and fluoride toothpaste, paying special attention to the gumline around your treated tooth. Flossing at least once a day is equally important, as it removes plaque and debris from between your teeth and below the gumline where your toothbrush can’t reach. Consider using an antiseptic mouthwash to reduce bacteria in your mouth and help prevent gum disease. If your root canal-treated tooth has a crown, be sure to clean carefully around the margins where the crown meets your natural tooth, as this area is particularly susceptible to decay.
Regular Dental Check-ups and Their Importance
Regular dental check-ups are essential for monitoring the health of your root canal-treated tooth. Visit your dentist every six months for professional cleanings and examinations. During these visits, your dentist will:
- Check the integrity of your restoration (filling or crown)
- Look for signs of decay around or under the restoration
- Assess the health of the surrounding gum tissue
- Take periodic X-rays to evaluate the bone around the root tip
- Check for any signs of fracture or other complications
These routine visits allow your dentist to identify and address potential problems before they become serious, significantly increasing the likelihood that your root canal-treated tooth will last a lifetime.
Dietary Considerations for Treated Teeth
What you eat can impact the longevity of your root canal-treated tooth. While there are no specific dietary restrictions after root canal treatment, some considerations can help protect your restored tooth:
- Avoid extremely hard foods that could fracture the tooth, especially if it doesn’t have a crown
- Limit sugary and acidic foods and beverages that can promote decay around the restoration
- Be cautious with very sticky foods that could potentially dislodge a filling or temporary crown
- If you have a temporary crown, avoid chewing on that side of your mouth until the permanent restoration is placed
- Consider cutting hard foods like apples, carrots, and nuts into smaller pieces rather than biting directly into them
These simple dietary precautions can help protect your investment in root canal treatment and ensure the long-term health of your tooth.
Protective Measures: Night Guards and Sports Guards
Protective measures can significantly extend the life of your root canal-treated tooth. If you grind or clench your teeth (a condition known as bruxism), wearing a custom-fitted night guard can prevent excessive wear and potential fracture of your treated tooth. Similarly, if you participate in contact sports or activities with a risk of facial injury, wearing a sports guard is essential to protect all your teeth, including the root canal-treated one. These protective devices are relatively inexpensive compared to the cost of repairing or replacing a damaged tooth, making them a wise investment in your oral health.
The Lifespan of Root Canal Treated Teeth
The lifespan of a root canal-treated tooth varies depending on several factors, including the initial condition of the tooth, the quality of the root canal procedure, the type of restoration placed, and how well the tooth is maintained afterward. Statistics show that root canal-treated teeth have a high success rate, with approximately 85-95% lasting ten years or more when properly restored and cared for. Many last a lifetime with appropriate maintenance. Factors that can reduce the lifespan include poor oral hygiene, failure to place a crown when recommended, undetected cracks or fractures, and recurrent decay. By following your dentist’s recommendations for care and maintenance, you can maximize the likelihood that your root canal-treated tooth will serve you well for many years to come.
Advancements in Root Canal Treatment and Aesthetic Outcomes
The field of endodontics has evolved dramatically over the past few decades, with significant advancements in techniques, materials, and technology that have improved both the success rates and aesthetic outcomes of root canal treatments. These innovations have transformed root canal therapy from a procedure focused solely on eliminating infection to one that also prioritizes preserving the natural appearance of the tooth. Understanding these advancements can help patients appreciate the modern approach to root canal treatment and the improved results it offers.
Today’s root canal procedures bear little resemblance to those performed just a generation ago. Enhanced imaging technologies allow for more precise diagnosis and treatment planning, while improved instruments and techniques enable more thorough cleaning of the root canal system. Newer filling materials and restoration options have virtually eliminated the aesthetic concerns that once plagued root canal-treated teeth. These advancements mean that patients can now save their natural teeth without compromising their smile’s appearance, a win-win situation that wasn’t always possible in the past.
Modern Techniques for Better Aesthetic Results
Modern root canal techniques prioritize both function and aesthetics. One significant advancement is the use of operating microscopes, which allow endodontists to see inside the tooth’s canals at magnifications of up to 25 times. This enhanced visibility enables more thorough cleaning and shaping of the canals while preserving more of the natural tooth structure. Minimally invasive access techniques reduce the size of the opening needed to perform the procedure, helping to maintain the tooth’s structural integrity. Additionally, modern irrigation systems more effectively remove debris and bacteria from the canal system, reducing the risk of reinfection and subsequent discoloration. These techniques combine to produce better functional and aesthetic outcomes than traditional methods.
Materials That Improve Tooth Appearance Post-Treatment
The materials used in modern root canal treatments have been specifically developed to improve aesthetic outcomes. Traditional root canal filling materials sometimes contained components that could cause tooth discoloration over time. Today’s gutta-percha points and sealers are biocompatible and designed to minimize staining. For the access cavity, tooth-colored composite resins can be used instead of metal amalgam, creating a virtually invisible repair. When crowns are needed, all-ceramic options like zirconia and lithium disilicate provide excellent strength while mimicking the light-reflecting properties of natural teeth. These advanced materials ensure that root canal-treated teeth can blend seamlessly with your natural smile, eliminating the aesthetic concerns that once accompanied endodontic treatment.
Minimally Invasive Approaches to Root Canal Therapy
Minimally invasive approaches to root canal therapy focus on preserving as much of the natural tooth structure as possible, which directly benefits the aesthetic outcome. Traditional techniques often required significant removal of tooth structure to access and clean the canals. Modern approaches use smaller, more flexible instruments that can navigate curved canals with less removal of dentin. Ultrasonic tips allow for precise removal of calcifications and old filling materials with minimal impact on surrounding tooth structure. These conservative approaches maintain more of the tooth’s natural strength and reduce the risk of fracture, while also preserving the natural appearance by minimizing the need for extensive restorative materials.
Future Trends in Endodontic Treatments
The future of endodontic treatments promises even better aesthetic outcomes through emerging technologies and techniques. Regenerative endodontics, an exciting field of research, aims to regenerate the pulp-like tissue inside the tooth, potentially restoring some vitality and reducing the brittleness associated with traditional root canals. Three-dimensional imaging and guided surgery techniques may allow for even more precise and conservative treatments. Advanced biomaterials are being developed that can promote healing and regeneration of the surrounding tissues. Artificial intelligence is beginning to play a role in diagnosis and treatment planning, potentially improving success rates and outcomes. While many of these innovations are still in development or early adoption, they represent the future of root canal therapy—a future where saving a natural tooth doesn’t mean compromising its appearance.
Frequently Asked Questions
Q: Will my tooth look different after a root canal?
A: In most cases, your tooth will look very similar to how it did before the root canal, especially once it’s been properly restored. The external appearance typically doesn’t change significantly, though some teeth may develop slight discoloration over many years. With modern techniques and materials, this is becoming less common, and any aesthetic concerns can usually be addressed with appropriate restorative options.
Q: Why do some teeth turn dark after root canal treatment?
A: Tooth discoloration after root canal treatment can occur for several reasons. Historically, some root canal filling materials contained components that could stain the tooth from the inside. Additionally, the breakdown of blood products that were present in the tooth before treatment can cause internal staining. However, modern techniques and materials have largely eliminated these issues, and if discoloration does occur, it can often be corrected with internal bleaching, veneers, or crowns.
Q: How long will a root canal-treated tooth last?
A: With proper care and restoration, root canal-treated teeth can last a lifetime. Studies show success rates of 85-95% at ten years post-treatment. The longevity depends on factors including the initial condition of the tooth, the quality of the root canal procedure, the type of restoration placed, and how well the tooth is maintained through good oral hygiene and regular dental check-ups.
Q: Is a crown always necessary after a root canal?
A: While not absolutely mandatory in all cases, crowns are highly recommended for most root canal-treated teeth, especially posterior teeth that endure significant chewing forces. After root canal treatment, teeth become more brittle and prone to fracture. A crown provides essential protection by covering and strengthening the entire tooth structure. For anterior teeth, depending on the amount of remaining healthy tooth structure, more conservative restorations like porcelain veneers might be considered in some cases.
Conclusion
Understanding what a tooth looks like after root canal treatment is essential for anyone undergoing or considering this common dental procedure. As we’ve explored throughout this comprehensive guide, modern root canal therapy has evolved to prioritize both function and aesthetics, allowing patients to save their natural teeth while maintaining a beautiful smile. The external appearance of a properly treated and restored tooth should be virtually indistinguishable from your natural teeth, with no visible evidence of the internal treatment that has taken place.
The journey of a tooth through root canal treatment involves significant internal changes while preserving its external appearance. By removing infected or damaged pulp and replacing it with biocompatible materials, endodontists can eliminate pain and infection while maintaining the tooth’s structure. When followed by appropriate restoration—typically a crown for posterior teeth or a more conservative restoration for anterior teeth—the result is a functional, natural-looking tooth that can serve you well for many years to come.
It’s important to remember that the success of root canal treatment depends not only on the skill of your dental provider but also on your commitment to proper aftercare and maintenance. Regular dental check-ups, good oral hygiene practices, and protective measures when needed all contribute to the long-term success of your treatment. By being an active participant in your oral healthcare, you can ensure that your root canal-treated tooth remains both functional and aesthetically pleasing for years to come.
If you’ve been putting off needed root canal treatment due to concerns about appearance or misconceptions about the procedure, take comfort in knowing that modern endodontics offers excellent outcomes both in terms of function and aesthetics. Saving your natural tooth is always preferable to extraction when possible, and with today’s advanced techniques and materials, you don’t have to choose between oral health and a beautiful smile.